COMISA: How to Manage Insomnia and Sleep Apnea Together
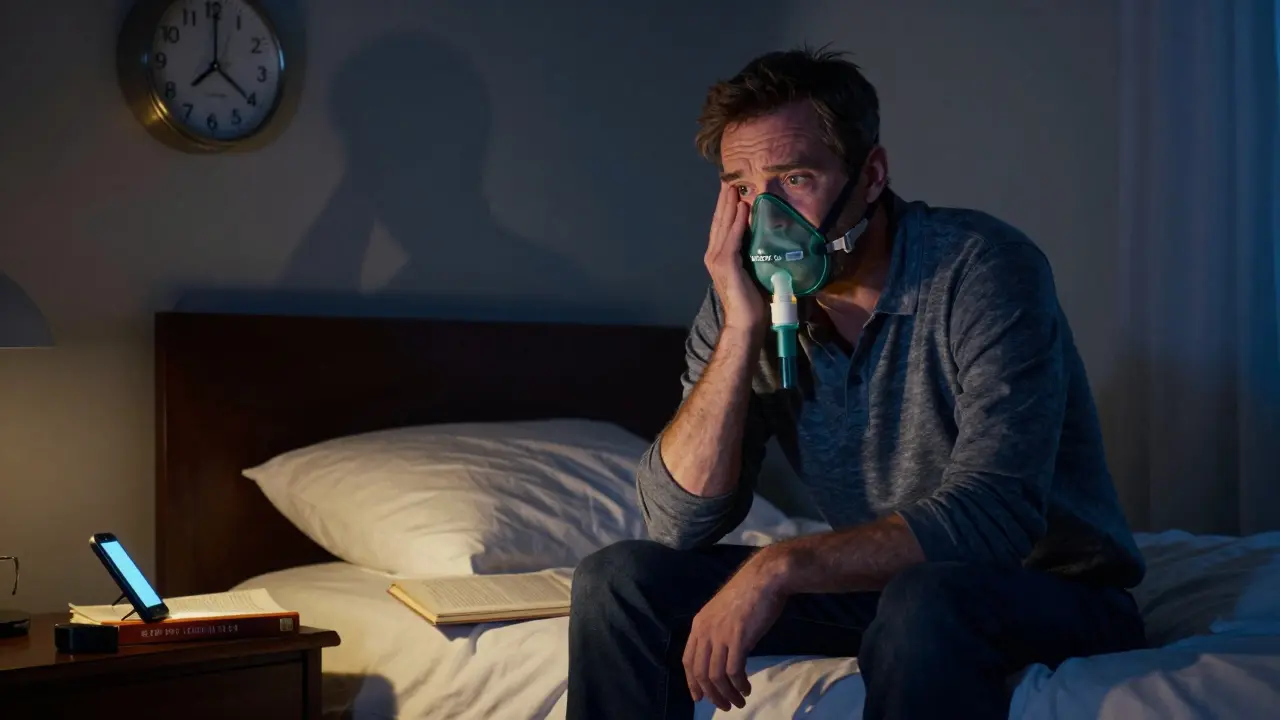
Imagine lying awake at 3 a.m., heart pounding, thinking about the CPAP mask digging into your face. You’ve been using it for weeks, but sleep still feels broken. You’re not alone. Between 39% and 58% of people diagnosed with sleep apnea also struggle with chronic insomnia - a combo called COMISA. It’s not just two problems stacked on top of each other. It’s a tangled mess where one makes the other worse. And treating just one? That often fails.
What Is COMISA, Really?
COMISA stands for Comorbid Insomnia and Sleep Apnea. It’s when someone has both obstructive sleep apnea (OSA) - where breathing stops repeatedly during sleep - and insomnia, where falling or staying asleep is a constant struggle. This isn’t rare. In fact, it’s the most common sleep disorder combo you’ve never heard of.
Most doctors treat one condition at a time. First, they push CPAP for sleep apnea. Then, if you’re still tossing and turning, they suggest sleep hygiene tips or maybe medication for insomnia. But here’s the problem: CPAP can make insomnia worse. The mask feels claustrophobic. The air pressure wakes you up. The machine beeps. You start dreading bedtime. And if you’re already anxious about sleep, that fear grows.
Studies show that without treating insomnia, only 43% of COMISA patients stick with CPAP after six months. That’s not a failure of willpower. It’s a failure of the system. COMISA needs a different approach - one that fixes both problems at once.
Why Treating Just One Doesn’t Work
Let’s say you have sleep apnea with an AHI (Apnea-Hypopnea Index) of 22 - that’s moderate to severe. Your doctor gives you a CPAP machine. Great, right? But if you’re also struggling with sleep maintenance insomnia - waking up multiple times a night - CPAP alone won’t fix that. In fact, the noise, the mask, the pressure changes can trigger more awakenings.
On the flip side, if you only do CBT-I (Cognitive Behavioral Therapy for Insomnia), you’re still breathing poorly at night. Your body isn’t getting enough oxygen. Your heart is working harder. Your risk of high blood pressure, stroke, and heart disease stays high. You might sleep longer, but you’re not sleeping well.
Research from Flinders University shows that 39% of OSA patients still report insomnia even after months of CPAP use. That’s not a coincidence. It’s the nature of COMISA. The two conditions feed each other. Poor sleep from insomnia makes your airway more collapsible. Breathing interruptions from apnea make your brain hyper-alert, so you can’t relax enough to fall asleep.
The Only Proven Solution: CBT-I + CPAP Together
The only treatment proven to work for COMISA is doing both CBT-I and CPAP at the same time - not one after the other, but side by side.
CBT-I isn’t just counting sheep or drinking chamomile tea. It’s a structured, evidence-based program that changes how you think and behave around sleep. It includes:
- Stimulus control: Only use your bed for sleep and sex. No scrolling, no reading, no watching TV in bed.
- Sleep restriction: You spend less time in bed to build up sleep pressure. It sounds counterintuitive, but it works.
- Cognitive restructuring: Challenging thoughts like “I’ll never sleep” or “If I don’t sleep 8 hours, I’ll collapse tomorrow.”
- CPAP-specific adaptations: Learning to tolerate the mask, adjusting to airflow, managing anxiety around the machine.
A 2020 randomized trial found that when CBT-I was combined with CPAP from day one, 63% of COMISA patients saw their insomnia go into remission after 12 weeks. With CPAP alone? Only 29%.
And the CPAP usage? Patients using both treatments added an extra 1.2 hours of use per night. That’s not just better sleep - that’s lower risk for heart disease, better mood, sharper focus during the day.

Who Should Get This Treatment?
Not everyone with insomnia and apnea needs the full combo. But if you meet these criteria, you’re likely a candidate:
- You’ve been diagnosed with OSA (AHI ≥ 5) and insomnia (ISI score ≥ 15)
- You’ve tried CPAP but stopped using it because you couldn’t sleep
- You’ve tried sleep hygiene or medication for insomnia and it didn’t stick
- You wake up frequently at night, even with CPAP on
- You feel anxious or frustrated about sleep
There’s one big catch: you need access to both a sleep physician and a psychologist trained in CBT-I. That’s not easy. In the U.S., only 12% of COMISA patients have access to a CBT-I specialist. Wait times can be 14 weeks or more.
But digital CBT-I platforms are changing that. Apps like Sleepio and Somryst now include modules specifically designed for COMISA. They track your CPAP usage and adjust CBT-I strategies accordingly. Studies show they work well for mild to moderate cases. But if your AHI is above 15, you still need in-person support.
The Hidden Barriers - And How to Beat Them
Even when you know what to do, getting there is hard.
Cost: A full course of CBT-I can cost $1,200-$1,800. CPAP machines run $800-$3,000. Insurance often covers the machine, but not always the therapy. That’s changing. In January 2024, Medicare started reimbursing for integrated COMISA treatment with new billing codes (G2212-G2214). If you’re in the U.S., ask your provider about these codes.
Coordination: Most sleep centers don’t talk to psychologists. You get handed a CPAP machine and told to call back in six weeks. That’s not care - that’s a transaction. Look for clinics with “integrated sleep programs” or “sleep navigators” - staff who coordinate between your doctor and therapist. Mayo Clinic, Stanford, and some VA hospitals have them.
Mask discomfort: This is the #1 reason people quit CPAP. Try different masks - nasal pillows, full face, hybrid. Use a ramp feature that slowly increases pressure. Try a humidifier. And if you’re still struggling, don’t give up. CBT-I can help you reframe the discomfort as temporary, not unbearable.
Underlying trauma: About one-third of COMISA patients have trauma-related insomnia. If you’ve been through something life-changing - accident, abuse, loss - your insomnia might need special CBT-I techniques. Ask your therapist if they’ve worked with trauma survivors.
What About Other Treatments?
You might hear about other options: mandibular devices, neurostimulation, or drugs like suvorexant.
Mandibular advancement devices help mild to moderate OSA, but they don’t fix insomnia. Neurostimulation (like Inspire) is for severe OSA patients who can’t use CPAP - but again, it doesn’t touch insomnia.
Suvorexant, a new FDA-approved drug for COMISA, helps you fall asleep faster. In trials, it improved sleep maintenance by 42%. But it’s not a cure. It’s a band-aid. And it can cause next-day drowsiness. It’s best used short-term while you build habits with CBT-I.
None of these replace the combo of CBT-I and CPAP. They’re alternatives for people who can’t access the gold standard - not replacements for it.

What’s Next for COMISA?
Things are changing fast. A 2023 study from Flinders University used machine learning to predict who will respond best to combined treatment - with 78% accuracy. That means in the near future, your doctor might use your sleep data, anxiety levels, and breathing patterns to decide if you’re a CBT-I candidate.
ResMed’s new AirSense 11 adjusts pressure based on your sleep stage. If you’re in deep sleep, it lowers pressure. If you’re waking up, it stabilizes. That’s huge for COMISA patients who get jolted awake by sudden pressure changes.
And insurance? UnitedHealthcare found that COMISA patients on combined treatment used 22% fewer healthcare services - ER visits, doctor appointments, medications - saving $1,843 per person per year. That’s why payers are starting to fund integrated programs.
But the biggest barrier isn’t technology. It’s awareness. Most primary care doctors still treat insomnia and sleep apnea as separate problems. They don’t know COMISA is a distinct diagnosis. If you’ve been told you have “just insomnia” or “just sleep apnea” and nothing’s improving - ask for a sleep study with insomnia screening. Push for CBT-I. You’re not being difficult. You’re being smart.
Real People, Real Results
One man from Ohio, 58, had CPAP for 18 months. He used it 2 hours a night. He felt exhausted. He was irritable. His wife left him.
He joined a program that paired CBT-I with CPAP coaching. He learned to use the mask only when he was ready to sleep. He stopped checking the clock. He stopped forcing himself to sleep. Within eight weeks, he was using CPAP 6.7 hours a night. He got his wife back.
A woman in Florida, 42, had insomnia since her divorce. She was diagnosed with OSA a year later. She tried sleeping pills. They made her groggy. She tried CPAP. It made her panic. She started CBT-I and CPAP together. After three months, she slept through the night. She stopped taking pills. She started running again.
These aren’t outliers. They’re the norm - when the right treatment is used.
What You Can Do Today
If you think you have COMISA, here’s your action plan:
- Get a sleep study (polysomnography) that measures both breathing and sleep quality - not just apnea events.
- Ask for the Insomnia Severity Index (ISI). If your score is 15 or higher, you have clinical insomnia.
- Ask your doctor: “Do you treat COMISA with CBT-I and CPAP together?” If they say no, ask for a referral to a behavioral sleep specialist.
- If you can’t find one, try a digital CBT-I platform like Sleepio or Somryst - but only if your AHI is under 15.
- Don’t give up on CPAP. Use a ramp feature. Try a different mask. Use a humidifier. And pair it with CBT-I.
You don’t have to live with broken sleep. COMISA is hard - but it’s treatable. The tools exist. The evidence is solid. You just need to ask for the right kind of help.
Is COMISA the same as having insomnia and sleep apnea separately?
No. COMISA is a distinct clinical condition where insomnia and sleep apnea interact and worsen each other. Treating them separately often fails because the two conditions feed off each other. For example, CPAP can trigger insomnia symptoms, and insomnia can make breathing events worse. COMISA requires a combined treatment approach.
Can I just use a CPAP machine and ignore my insomnia?
Probably not. Studies show that 39% of people with sleep apnea still have insomnia even after using CPAP. Without addressing the insomnia, CPAP adherence drops to under 43% after six months. You might reduce your breathing events, but you won’t feel rested - and you’re at higher risk for dropping out of treatment entirely.
Is CBT-I effective for people who use CPAP?
Yes - and it’s even more effective when combined with CPAP. A 2020 trial found that 63% of COMISA patients achieved insomnia remission with CBT-I and CPAP together, compared to only 29% with CPAP alone. CBT-I helps you tolerate the mask, reduce anxiety around sleep, and build consistent routines that make CPAP easier to use.
How do I find a therapist who treats COMISA?
Look for sleep specialists certified in CBT-I. Ask your sleep doctor for a referral. Check the website of the Society of Behavioral Sleep Medicine or the American Academy of Sleep Medicine. If you’re in the U.S., search for clinics with “integrated sleep programs” or “sleep navigators.” Digital CBT-I platforms like Sleepio and Somryst are good alternatives if in-person care isn’t available.
Will insurance cover CBT-I for COMISA?
It’s getting better. Since January 2024, Medicare in the U.S. has added specific billing codes (G2212-G2214) for integrated COMISA treatment, reimbursing $125-$185 per session. Many private insurers are following suit. Ask your provider if they accept these codes. Even if they don’t, CBT-I is often covered under mental health benefits - call your insurance to confirm.
Can digital CBT-I replace in-person therapy for COMISA?
For mild to moderate COMISA (AHI under 15), digital CBT-I works well and improves CPAP adherence. But for severe OSA (AHI over 15), in-person support with a trained therapist is still recommended. Digital tools can’t adjust to complex cases like trauma-related insomnia or severe mask anxiety. Use them as a bridge - not a substitute - if access is limited.
How long does it take to see results with CBT-I and CPAP?
Most people start noticing improvements in sleep quality and CPAP use within 4-6 weeks. Full remission of insomnia symptoms typically takes 8-12 weeks. CPAP adherence increases steadily over time - especially when paired with CBT-I. Don’t expect overnight change. But with consistency, most people report feeling like they’ve gotten their life back.
kenneth pillet
January 18, 2026 AT 11:44Stop treating them like separate problems. They’re a team. Fight them together.
Naomi Keyes
January 20, 2026 AT 08:11Jodi Harding
January 21, 2026 AT 23:43Robert Cassidy
January 23, 2026 AT 19:28Kristin Dailey
January 24, 2026 AT 09:00Aysha Siera
January 24, 2026 AT 10:56Wendy Claughton
January 24, 2026 AT 20:04Stacey Marsengill
January 24, 2026 AT 22:18Zoe Brooks
January 25, 2026 AT 20:32