How Colitis Affects Focus and Memory: What You Need to Know
Colitis & Cognitive Symptoms Tracker
Based on your current status, here's how your symptoms might affect your daily activities:
- Stay hydrated - aim for 2-3 liters of water daily
- Log meals and brain-fog episodes to identify patterns
- Schedule short mental breaks every 45 minutes of screen work
- Include omega-3 rich foods (salmon, chia seeds) daily
- Practice 5-minute breathing exercises before bed
When discussing chronic gut disorders, Colitis is a type of inflammation that targets the lining of the large intestine. It can range from mild irritation to severe ulceration, often causing abdominal pain, diarrhea, and urgent bowel movements. While the digestive symptoms are obvious, many patients don’t realize how the inflammation can seep into the brain, messing with colitis and memory and overall mental focus.
Key Takeaways
- Inflammation in the gut triggers chemical signals that influence the brain’s attention and memory circuits.
- Common cognitive complaints include brain fog, shorter attention span, and difficulty recalling recent events.
- Gut‑brain axis disruptions, elevated cytokines, and stress hormones are the main culprits.
- Diet, stress management, and tailored medication can lessen the mental side‑effects.
- If cognitive issues worsen or interfere with daily life, a healthcare professional should evaluate you promptly.
What Is Colitis?
Colitis falls under the broader umbrella of inflammatory bowel disease (IBD). The two most common forms are ulcerative colitis, which is limited to the colon, and Crohn’s disease, which can affect any part of the gastrointestinal tract but often involves the colon as well. Typical triggers include genetic predisposition, immune system misfires, and environmental factors such as diet or smoking. Diagnosis usually involves colonoscopy, blood tests for inflammatory markers, and stool analysis.
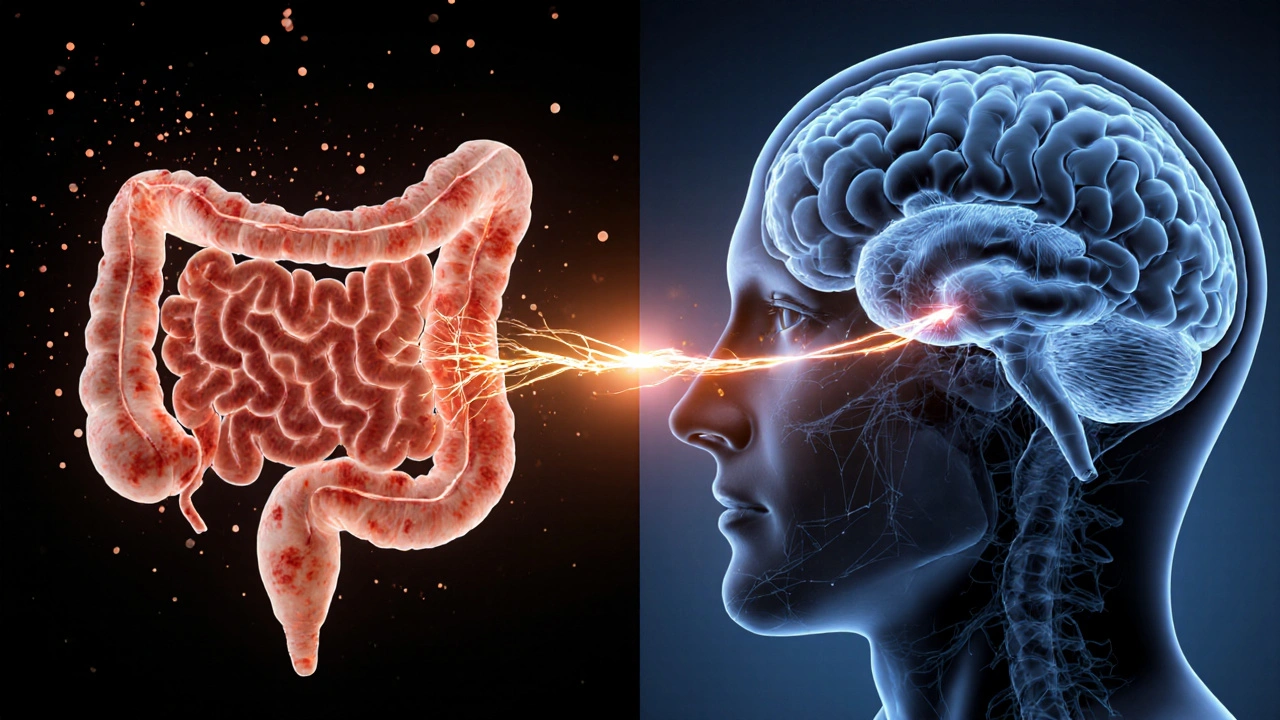
The Gut‑Brain Connection
Enter the Gut‑brain axis - a two‑way communication highway linking the digestive tract and the central nervous system. This axis relies on three main messengers:
- Neural pathways, especially the vagus nerve.
- Hormones such as cortisol, released during stress.
- Immune signals, notably cytokines small proteins that coordinate inflammation
When colitis flares, the gut’s immune cells pump out cytokines like interleukin‑6 (IL‑6) and tumor necrosis factor‑α (TNF‑α). These molecules don’t stay confined to the gut; they circulate, cross the blood‑brain barrier, and alter neurotransmitter balance. At the same time, an imbalance in the microbiome the community of trillions of gut bacteria can produce metabolites that either soothe or aggravate brain inflammation.
How Inflammation Impacts Focus
Focus, or sustained attention, depends on a well‑orchestrated network involving the prefrontal cortex, dopamine, and acetylcholine. Cytokines can interfere with dopamine production, leading to slower reaction times and a pervasive sense of “brain fog.” Moreover, elevated cortisol during a flare spikes the body’s fight‑or‑flight response, causing the hippocampus (the brain’s memory hub) to work less efficiently. The result? Forgetting where you placed your keys, missing deadlines, or needing to reread the same paragraph multiple times.
Memory Impairment Explained
Memory is split into short‑term (working) memory and long‑term consolidation. Studies from 2023‑2024 show that IBD patients score 15‑20% lower on standard working‑memory tests compared with healthy controls. The culprit is often the same cytokine cocktail that disrupts focus, but it also hampers the hippocampus’s ability to encode new information. Chronic inflammation can even accelerate age‑related memory decline, a concern for patients diagnosed in their twenties.

Real‑World Signs to Watch For
If you’ve been diagnosed with colitis, keep an eye on these cognitive red flags:
- Sudden difficulty concentrating during a flare.
- Frequent “I can’t remember what I just read” moments.
- Increased forgetfulness about appointments or medication schedules.
- Feeling mentally exhausted after a short period of mental work.
- Heightened anxiety or low mood that seems tied to gut symptoms.
Managing Cognitive Side‑Effects
While you can’t fully control the immune system, you can influence the signals that travel to the brain.
Dietary Tweaks
- Increase omega‑3 rich foods (salmon, chia seeds) to help modulate cytokine production.
- Limit processed sugars and alcohol, both of which can spike inflammation.
- Consider a low‑FODMAP diet under dietitian supervision to reduce gut irritation.
Stress‑Reduction Practices
- Mindful breathing for 5‑10 minutes daily lowers cortisol.
- Gentle yoga or tai‑chi supports vagal tone, strengthening gut‑brain signaling.
Medication Review
Some drugs used for colitis, like corticosteroids, can worsen mood and memory short‑term. Biologic agents (e.g., anti‑TNF treatments) often reduce systemic inflammation and, indirectly, brain fog. Talk to your gastroenterologist about balancing gut relief with cognitive health.
Physical Activity
Regular moderate exercise boosts blood flow to the brain, aids neurogenesis, and helps regulate gut motility. Aim for 150 minutes of brisk walking, cycling, or swimming each week.
When to Seek Professional Help
If cognitive symptoms persist beyond a flare, interfere with work or studies, or are accompanied by severe mood swings, it’s time to involve both a gastroenterologist and a neurologist or psychologist. They may order blood tests for cytokine levels, neurocognitive assessments, or even MRI scans to rule out other causes.
Comparison of Common Cognitive Symptoms in Colitis Patients
| Symptom | Active Flare (% of patients) | Remission (% of patients) | Typical Trigger |
|---|---|---|---|
| Brain fog | 68 | 22 | Elevated cytokines, dehydration |
| Short‑term memory lapses | 54 | 15 | High cortisol, sleep disruption |
| Difficulty concentrating | 61 | 19 | Fatigue, medication side‑effects |
| Increased anxiety | 45 | 12 | Gut‑brain axis dysregulation |
Quick Checklist for Daily Brain Health
- Stay hydrated - aim for 2‑3L of water a day.
- Log your meals and any brain‑fog episodes; patterns can guide treatment.
- Schedule short mental breaks every 45minutes of screen work.
- Include at least one omega‑3 serving daily.
- Practice a 5‑minute breathing exercise before bed.
Frequently Asked Questions
Can colitis cause permanent memory loss?
Most memory problems are reversible once inflammation subsides. Chronic, unmanaged inflammation, however, can accelerate age‑related decline, so early treatment is key.
Are certain medications worse for focus?
Corticosteroids can cause jitteriness and sleep disturbances, which hurt concentration. Biologics that reduce systemic inflammation often improve cognitive clarity.
How long does brain fog last after a flare?
It varies. Most people feel improvement within 1‑3 weeks once bowel symptoms are under control, but some may need months of lifestyle adjustments.
Do probiotics help with mental focus?
Certain strains (e.g., Bifidobacterium longum) have shown modest benefits for mood and cognition, especially when paired with a low‑FODMAP diet.
Should I see a neurologist for colitis‑related brain issues?
If cognitive symptoms persist despite gut‑focused treatment, a referral to a neurologist or neuropsychologist can provide targeted assessments and coping strategies.
josue rosa
October 5, 2025 AT 01:44The interplay between mucosal immunology and neurocognitive pathways is profoundly intricate, especially when one considers the cytokine-mediated disruption of the hypothalamic-pituitary-adrenal axis during colitic exacerbations. Elevated interleukin‑6 and tumor necrosis factor‑α act as neuroactive messengers that can traverse the compromised blood‑brain barrier, thereby impeding dopaminergic transmission in the prefrontal cortex. This biochemical milieu fosters the quintessential "brain fog" that patients frequently report, characterized by attenuated working memory and diminished attentional capacity. Moreover, sustained glucocorticoid exposure during flares precipitates hippocampal neurogenesis inhibition, which further compromises episodic memory consolidation. Recent neuroimaging studies have demonstrated reduced functional connectivity in the default mode network among individuals with active ulcerative colitis, corroborating the clinical phenomenology of cognitive sluggishness. Dietary constituents such as omega‑3 polyunsaturated fatty acids have been shown to exert anti‑inflammatory effects that may ameliorate these neurocognitive sequelae by modulating microglial activation. Conversely, high glycemic load meals exacerbate systemic inflammation, potentially amplifying cytokine spillover into central nervous tissue. It is also imperative to recognize the bidirectional nature of the gut‑brain axis; heightened psychological stress can aggravate intestinal permeability, setting up a vicious feedback loop. In clinical practice, a multimodal approach that integrates dietary modification, stress‑reduction techniques, and judicious pharmacotherapy yields the most favorable outcomes for cognitive symptom mitigation. Patients are encouraged to maintain meticulous symptom diaries to identify specific triggers and to discuss these patterns with their gastroenterology team. Ultimately, addressing the inflammatory substrate not only alleviates gastrointestinal distress but also restores neurocognitive homeostasis, enhancing overall quality of life.
Angie Wallace
October 7, 2025 AT 09:17Great overview, thanks for breaking it down.
Doris Montgomery
October 9, 2025 AT 16:51Honestly, seems like another excuse for people to claim "brain fog" without a real reason.
Nick Gulliver
October 11, 2025 AT 10:31Patriotic gut health is what we need.
Sadie Viner
October 13, 2025 AT 18:04Thank you for the comprehensive guide. I appreciate the formal tone and the inclusion of both dietary and psychological strategies. Being methodical about tracking symptoms can indeed reveal patterns that are otherwise hidden. It empowers patients to take an active role in their care, which is essential for chronic conditions.
Kristen Moss
October 15, 2025 AT 11:44Let’s not forget the American diet’s role.
Rachael Tanner
October 17, 2025 AT 19:17Fascinating how cytokine cascades can hijack neural circuits. The article nicely ties immunology to everyday cognitive lapses. I’d add that probiotic strains like Bifidobacterium longum have shown promise in modulating these pathways.
Debra Laurence-Perras
October 19, 2025 AT 12:57Spot on! Keeping a hopeful outlook while tracking can make a big difference. Stay optimistic and keep logging those episodes.
dAISY foto
October 21, 2025 AT 20:31Wow this is sooo helpful!! I never knew my gut could mess wit my memory. Keep logging and stay positive, we got this!!
Never underestimate the power of a good breather before bed.
Ian Howard
October 23, 2025 AT 14:11Indeed, integrating mindful breathing can reset the vagal tone. Try a 5‑minute session after each work block.
Chelsea Wilmer
October 25, 2025 AT 21:44The philosophical implications of the gut‑brain dialogue are profound, suggesting that our very identity is interwoven with microbial symbiosis. When inflammation spikes, the delicate equilibrium is disturbed, leading to a cascade of neurochemical disruptions that manifest as attentional deficits and memory lapses. This neuro‑immunological crosstalk is not merely a peripheral inconvenience but a central determinant of cognitive fidelity. Empirical data from recent longitudinal studies indicate that patients with persistent elevated C‑reactive protein exhibit measurable declines in executive function scores over a six‑month period. Moreover, the hippocampal atrophy observed in chronic IBD cohorts underscores the irreversible potential of unchecked inflammation. On a practical level, the adoption of a low‑FODMAP regimen coupled with omega‑3 supplementation has been associated with a statistically significant reduction in self‑reported brain fog. However, it is crucial to recognize that pharmacologic agents such as corticosteroids, while effective for acute flare control, may paradoxically exacerbate mood volatility and sleep disturbance, thereby compounding cognitive impairment. The solution lies in a balanced therapeutic strategy that leverages biologic agents to temper systemic cytokine production while minimizing neurotoxic side effects. Patients should also engage in regular aerobic exercise, which has been shown to promote neurogenesis and improve synaptic plasticity. Finally, a collaborative care model involving gastroenterologists, neurologists, and mental health professionals ensures a holistic approach to the multifaceted challenges presented by colitis‑related cognitive symptoms.
David Stout
October 27, 2025 AT 14:24Your synthesis is impressive and highlights the need for interdisciplinary care. Let’s keep pushing for integrated clinics.
Pooja Arya
October 29, 2025 AT 21:57One must question whether society truly values the invisible struggles of those with chronic illness. The narrative often marginalizes the mental toll, yet it is an undeniable component of holistic health. Let us champion a more compassionate discourse.
Sam Franza
October 31, 2025 AT 15:37Compassion over judgment, always.
Raja Asif
November 2, 2025 AT 09:17Enough with the fluff, get to the science already.